
Posts Tagged: diabetes
New research director at the Nutrition Policy Institute inspires positive change in human health

"Even more alarming," continued Crawford, "is a little known fact that 23 percent of the adolescents in this country currently have pre-diabetes or diabetes as measured by actual blood tests in our largest national study of health (NHANES). Something is seriously wrong in a society such as ours where so many children are growing up with such a high risk of preventable disease.”
The UC Food Observer published an extensive interview with Crawford, who, prior to joining the NPI, co-founded and directed the Center for Weight and Health at UC Berkeley for 15 years. She is a UC ANR Cooperative Extension nutrition specialist, as well as an adjunct professor in the School of Public Health at UC Berkeley.
Crawford led the 10-year longitudinal NHLBI Growth & Health Study, an epidemiologic study on the development of obesity in African American girls and FitWIC, the five-state obesity prevention initiative in WIC. She is currently leading studies evaluating a wide variety of state and national nutrition programs and policies. An internationally respected researcher, Crawford served on the California Legislative Task Force on Diabetes and Obesity and chaired the Institute of Medicine's Workshop (IOM) on Food Insecurity and Obesity.
Following is the UC Food Observer's Q&A with Pat Crawford:
Q: You have worked very hard over several decades to inspire positive change in human health. Can you tell our readers a little about the nutrition politics and the situation that encouraged you to do this? What keeps you passionate about your work?
A: From the 1970s to the 1990s, I was involved in research studies measuring the health effects of children's diets and physical activity levels, with particular attention to racial and ethnic disparities. Over this time period, I saw clear evidence of the deterioration of children's diets, with a disturbing and widespread transition to convenience foods and snack-type processed foods. These foods were being sold and distributed in the very institutions where children learned and were cared for. They were widely advertised and marketed to children and were replacing more nutritious foods. New foods were often heavily fortified, deceptively making them seem like nutritious alternatives. While I was watching these dietary changes, I also began to see the rapid, unprecedented, shocking rise in childhood obesity, with accompanying implications for health. We learned that childhood diets characterized by excessive calories from low-nutrient foods could lead to negative population-wide health effects during childhood as well as during adulthood. Our processed and snack-food rich diet was associated with a tripling in the rates of childhood obesity and a new spread of type 2 diabetes never before seen among children. I knew I needed to stop watching the trends and start trying to reverse them.
What keeps me passionate is knowing that change is possible when high quality policy relevant research is conducted and communicated to decision makers and those who work with children. During the last decade we have seen early signs of declines in the rapidly rising child obesity rates. If this energy to improve children's health continues for 20 more years, I would expect rates of child obesity to return to those in the years preceding the1980s, thereby nearly eliminating type 2 diabetes and heart disease risk factors in childhood.
A: This new unit is in the systemwide UC Division of Agriculture and Natural Resources, rather than being located on a specific campus. This provides more opportunities for multi-campus collaboration on issues that are of statewide and national concern. Being located in UC ANR, we also expect to use a broader food systems approach with a greater diversity of colleagues and, of course, utilize the power and reach of UC ANR Cooperative Extension to assure outreach throughout the state.
Q: People of color generally have poorer health outcomes in America. What public policies could help us change that? You led a seminal epidemiologic study on the development of obesity in African American girls. How does that work inform your thinking about nutrition education efforts and public policies in that arena?
A: The 10-year NHLBI Growth and Health Study was one of the first studies to disentangle the effects of race/ethnicity and family income and education on childhood obesity. We found that poverty is a critical determinant of obesity. This finding has guided my subsequent work conducting research on WIC [Women, Infants, and Children], the School Lunch Program, and SNAP-Ed [Supplemental Nutrition Assistance Program Education, previously food stamps], all of which provide an opportunity to address the most at-risk individuals, including children.
We have seen dramatic improvements in the programs. For example, the WIC program, which serves low-income pregnant women and their young children, revamped their food package to include more healthful foods. Similarly, new school lunch guidelines are assuring more healthful foods are served to children. Most of the children who benefit from this are low income students who qualify for free and reduced-price meals. There is still plenty of work to do to improve the programs, to ensure all those who could benefit have access to them, and that the benefits provided are funded adequately, but I am encouraged by how much has been accomplished.
Q: The average person knows relatively little about how research can inform and shape public policy. Are there insights you'd care to offer?
A: Policy-making bodies at both the state and national levels are eager to have science-based information to make the best decisions possible. Policymakers want to positively impact the health of their constituents. And more policymakers than ever are aware that our country spends far too much on healthcare and doesn't have the best health to show for it. This focuses increasing attention on disease prevention, as we clearly must do more to promote population health and keep people from needing to consume healthcare. Dietary intake is increasingly recognized as a major factor in the prevention and reduction of chronic disease rates in this country. Therefore, providing decisionmakers with good evidence about ways to improve dietary intake and thus population health offers opportunities to do something that helps constituents—and ultimately may lead to improvements in the nation's bottom line as well.
Q: The Academy of Nutrition and Dietetics recently received a great deal of negative attention when its new Kids Eat Right logo landed on Kraft Singles. They've had to walk back this decision, in part, due to pressure from their constituent group and folks like you. Any comments or insight you can provide on this situation? Is the logo a damaged brand now?
A: The Academy of Nutrition and Dietetics recently embarked on a new partnership with the food industry. However, it is my understanding that the Academy's membership questioned the terms of the partnership, thus bringing into question the degree of separation of nutrition professionals from the influence of industry. Food industry sponsorship of speakers at annual meetings of the dietetics profession is another example of action that has begun to cloud the Academy's reputation. If the Academy does not change its approach, I fear it could become a damaged brand.
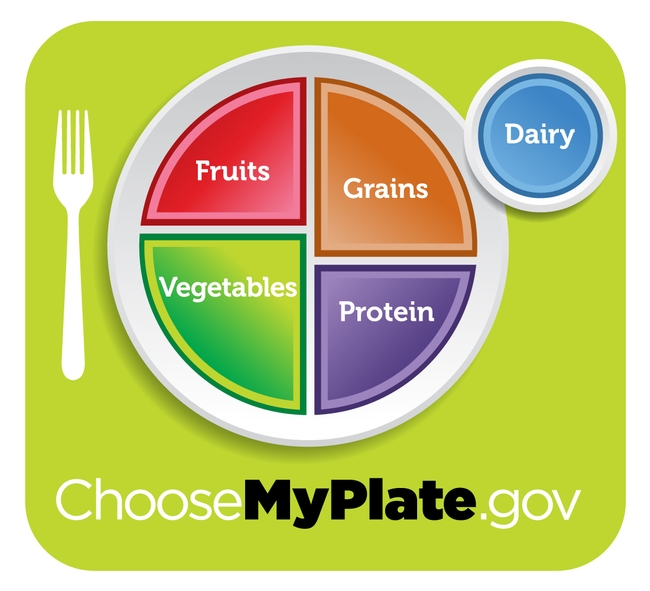
A: The Dietary Guidelines Advisory Committee is an independent scientific body that reviews the evidence behind the nation's dietary recommendations. The current evidence on dairy supports its inclusion in the recommendations. Thus, in my mind, the issue isn't the need for replacement of milk with water, but rather the replacement of soda, energy drinks, and other sugar-sweetened beverages with water. Hopefully educational materials for the public, including MyPlate, can begin to include water as the beverage that is first for thirst. Free water should be available in schools, childcare centers, worksites, public buildings and all other venues that serve children and adults.
Hopefully, the final Dietary Guidelines, when issued, will reflect the recommendation by the Dietary Guidelines Advisory Committee that added sugars be limited to no more than 10 percent of the calories in a diet. We have had strong evidence of sugar's contribution to diabetes, heart disease, obesity and dental caries. Therefore, in order for consumers to estimate their added sugar intake, it would be necessary for the FDA to modify the nutrition facts label to include added sugar. Without this information the American public has no resources with which to determine the amount of added sugar in their diet.
I also support the Committee's recommendation to consider sustainability when making dietary advice, and their encouragement of a plant-based diet. We are just beginning to understand all of the ways in which our food system is connected. Ensuring an adequate and adequately nourishing food supply for the population in the future demands that we continue to move in this direction.
Q: You're a researcher, but you also exert a profound influence in food politics. A battle is shaping up in Congress over the Healthy School Meals Act, which is due to expire at the end of September. In addition, the SNAP program is under fire by some politicians. Can you talk a little about the dynamics of these situations? Ultimately, what do you think might happen?
A: The safety net programs are under fire by some who seek to reduce or shift priorities in the federal budget, but the data overwhelmingly support the need for these programs for low-income Americans. We are spending more money on safety net programs now because so many people need them. In California, for example, more than half of our public school students qualify for free or reduced-price school meals and most babies born qualify for the WIC program. Thus, our food programs are not serving a small segment of our population but, rather, are necessary to sustain the majority of our population. We need to fix our economic challenges. In the meantime, cutting these food assistance programs would increase the risk for poor diets and the resultant long-term chronic disease costs, which would then paradoxically actually increase budgetary expenditures. Thus, cutting these programs would be an example of action that is penny-wise and pound-foolish.
Q: Can you tell our readers a bit about your most current research projects?
Q: Fomenting change is risky. What keeps you going when things get tough?
What keeps me going is the realization that we, as adults, are not adequately protecting our children. For a long time, we bought into the mantra that children were to blame for not making healthy food choices. We now have overwhelming evidence that children will make unhealthy choices only if given unhealthy food options; conversely, children will make healthy choices if given healthy food options. Adults are responsible for the health, well-being and protection of their children and this means provision of healthy food choices and lack of access to unhealthy food choices. Healthy food consumption is the single biggest factor for preventing chronic disease risk in children. Healthy food for children is an investment in our nation's future as surely as is education.
Q: Many are using social technologies for movement building in your profession (the work of the SugarScience team is just one example).

Q: Your work has a strongly ethical aspect to it. Are there unique challenges that nutrition professionals face in a free market environment?
A: Nutrition professionals have to contend with the enormous power of large multi-national corporations in the food industry. The power of food companies to influence policymakers cannot be overestimated, particularly when it comes to changing nutrition policies for our nation's food programs or trying to establish new policies to limit consumption of products we know are contributing to ill health. Further, the food industry has enormous resources available to market and promote foods and beverages with little or no nutritional value to children. This overwhelms and undermines the efforts of the limited nutrition education that is available to educate them. The free market fails here — consumers aren't able to get the information they need to make good decisions, and the people who profit from selling ill health are not the same ones who pay the consequences. Thus, it is up to those of us working in this area to make sure we share good information and work to change the systems that currently enable selling ill health to be so profitable.
Q: With a proliferation of labels, many consumers are confused. Do labels help someone concerned with ethical and environmentally aware eating?
A: Food companies make claims for their products, both in advertising and on the front of package labels that are deceptive and misleading. For example, a product may claim to have no gluten or no cholesterol despite the fact that that type of product never included those constituents. Products that say “lower salt” are often still very high in sodium. Some products claim to provide energy when they are really only indicating that the product provides calories. Confusion is commonplace.
Access to information on the environmental impact of food production is sorely limited. Only recently has the selection of a diet good for both the individual and for the planet become a part of our discourse. For people who can afford to shop at specialty food stores or farm stands, there are some suppliers in the marketplace that try to sell better choices in terms of environmental impact. But we have barely begun to do what is needed to support wide availability of dietary choices that are optimal for human or environmental health.
Q: Everyone gets the drought question! The California drought impacts the nation and the world. What changes might it bring about in the nation in terms of thinking about where and what we produce? What might the future hold for California, and agricultural production in the state?
A: There is much we don't know. Climate scientists and agricultural scientists are working to identify and predict the impact of various aspects of climate change including increased CO2 emissions, warming, and drought on crop yields and nutrient composition of various commodities. What I can say is that if the yields of fresh fruits and vegetables drop considerably, as they may do, we will have a grave situation. Fruit and vegetable intake by Americans is already inadequate. Eating enough affordable fruits and vegetables is going to be harder than ever, particularly for low-income Americans. This is yet another reason why reducing federal nutrition assistance programs at this time, as some are proposing, is not wise.
Q: What keeps you up at night?
A: I'm most worried that some of the progress we've made on policies to improve the healthfulness of school meals will be reversed due to political pressures based on the costs of healthy foods compared to the lower costs of less healthy foods, and the resistance of some to accept change that is in the best interest of children, particularly when it affects the profits of adults. I am also worried that there will be enormous lobbying efforts on behalf of less healthy foods that have been excluded from the new regulations. School meals should be more fully supported in order to provide children with the foods they need to be healthy.
Q: What might it take to get the next generation inspired to be concerned about nutrition and food policy?
A: I'm really pleased that these issues continue to be in the public eye and in the media. I hope that food and nutrition education will be reinstated in schools with the knowledge that this type of education can be provided in a way that it does not negatively impact test scores in common core subject areas. Currently children in the United States receive an average of only four hours of nutrition education a year, similar to the amount of time students are exposed to junk food advertising in a single week. With even modest increases in annual hours of food and nutrition education, I believe the next generation will be more aware and concerned about the relationship among nutrition, disease and food policy. We are seeing that the millennial generation is more interested in food issues than the generations before them, and this I find very encouraging.
Q: What must institutions and groups do to effect change in the food system?
A: I am heartened by the increased attention being focused on the food environment, policy and systems. A complex issue such as the food system requires input on multiple levels from multiple stakeholders. An example of the kind of effort that is needed is already underway on the University of California campuses. Last year, President Napolitano began the Global Food Initiative to harness the expertise and resources across multiple disciplines the UC system to address healthy and sustainable food systems.
Q: We're faced with challenges on a variety of fronts that have strongly ethical aspects to them, such as climate change, environmental constraints, income inequality, and food access. How do we get groups to move forward together? And is this a movement? How does the work of professional nutritionists fit into the larger food movement?

Q: I'm giving you a super power. You can change one thing about the food system with that super power. What change would you make?
A: I would level the playing field by reducing the influence of money to reduce the healthfulness of children's diets, both in the marketing of unhealthy foods to children, and in food industry lobbying of policy makers.
How do we get better food in our schools?
According to FoodCorps, only 2% of children eat enough fruits and vegetables. Kids in the south suffer from very high rates of obesity. 1 in 3 children born in 2000 are on track to develop type II diabetes and 50% of children of color are expected to develop diabetes during their lifetimes. That's an astounding number.
So how do we fix this? Debra Eschmeyer of FoodCorps (and speaker at California Roots, Global Reach) says we start with the schools.
Watch her video to see how:
Polluted air may contribute to farmworkers diabetes risk
The Sacramento Bee picked up on a UC news release about the most recent issue of California Agriculture journal, which said more than 1 million California farmworkers face a higher risk of diabetes and respiratory disease because of poor air quality.
The news release says California's Central Valley has the highest recorded levels of particulate matter in the country. The polluted air results in increased rates of asthma and other respiratory illnesses. In addition, the release said research points to possible environmental links between pesticide exposure and the risk of diabetes.
In a sample of 1,300 Mexican Americans who participated in the Hispanic Health and Nutrition Examination Survey, conducted from 1982 to 1984, higher levels of organochlorine compounds, which are found in pesticides, were observed in the blood of adults with self-reported diabetes compared to those without diabetes, according to the Cal Ag article.
"However, due to the cross-sectional design of the study, it is not clear whether there is a causal relationship between pesticide exposure and diabetes, or what the nature of that relationship may be," according to the article.
That said, perhaps the Sacramento Bee headline - "Farmworker diabetes risk linked to bad air" - is overstated.
The UC release also appeared on Yubanet.com.
The January to March issue of California Agriculture journal.
